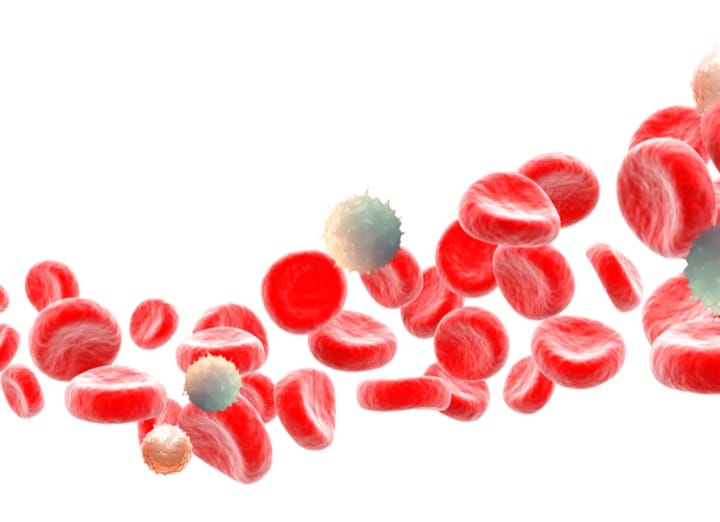
In the case of Immflamatory Bowel Disease (IBD), although other cells such as lymphocytes and monocytes have a certain role, the main inflammatory cells involved in the pathogenic mechanism are neutrophils, white blood cells, also called granulocytes.
Neutrophils are actively recruited from the bloodstream into the mucous layer of the intestine, causing the typical lesions of this disease through their degranulation and the release of various proteinases and chemokines.
In fact, the neutrophil’s significance in this disease is such that several studies have shown a strong correlation between the presence of neutrophils in the gastrointestinal wall of patients with IBD and the risk of clinical relapse (disease “flare-up”) or colon cancer.
Another fact that demonstrates the relevance of neutrophil presence in the intestinal linen of patients with IBD is the utility of faecal calprotectin measurement regarding the prediction of relapses or the diagnosis of disease activity even in the absence of symptoms. Faecal calprotectin is the main protein in the cytoplasm of neutrophils and is detectable in stools, as long as the intestinal tract mucosa is infiltrated by neutrophils. The physicochemical characteristics of this protein and its resistance to degradation by bacteria of the colon have allowed its use in clinical practice, making it the most used and reliable parameter for the management and evaluation of patients with IBD, specially with UC.