Inflammatory bowel disease (IBD) is a group of chronic inflammatory disorders affecting the intestine and/or other organs among which we can highlight, mainly: Crohn’s disease and ulcerative colitis. Both present a similar symptomatology that frequently manifests with abdominal pain, diarrhoea, isolated bleeding, blood in the stool (rectorrhagia), weight loss, among other symptoms.
Author: Adacyte
News
The emotional impact of having inflammatory bowel disease (IBD)
September 18, 2024
Patient

Due to this symptomatology and the chronic nature of the disease, with moments of flare-up and remission, these pathologies have an effect at an emotional level. Especially in times of flare-up, the symptoms have a direct impact on patients’ general well-being, as they see their physical condition affected and, therefore, their autonomy to carry out certain daily activities at a family, social and professional level. However, even patients with controlled symptoms report a clear impact in one or more of these areas.
Emotional support and IBD
According to one study 2, most patients believe that IBD has a negative psychological impact and that their disease worsens when they feel anxious (82%) or depressed (67%). More than half of patients feel sad or depressed (58%) or have anxiety (51%) at some point during the course of their disease. Most doctors (80%) agree that psychological aspects have an influence, so it is essential to maintain good emotional health to improve the course of the disease.
The social impact of IBD
IBD also imposes an additional burden on the social, professional and family life of those who suffer from it. They report impacts at the level of relationships with family or friends or in leisure and recreational activities. It also has an impact at a professional level, conditioning their work, the acceptance of promotions or even, in some rare cases, the loss of their job.
In younger patients, academic difficulties are reported, as well as problems finding a job.
The impact of IBD on sexuality3
As with any disease we suffer from, if we are not physically or emotionally well, our sexuality3 (broadly understood) may be affected.
It is true that, IBD, since it usually appears in adolescence and/or in young adults, can have a greater impact on the development of our sexuality. At this age, body image, self-esteem and personal relationships are of great importance, and IBD could affect full sexual development by causing decreased libido, body image concerns, anxiety or stress, especially in cases where there is a stoma or ileostomy.
Patients consider that suffering from IBD has caused a decrease in libido (almost 50%), prevents them from continuing intimate relations (45%), is associated with the break-up of a relationship (36%) or worsening of sexual activity (> 35%) and has made them choose abstinence, especially during the active phase of IBD (67%) but also during remission (19%). Patients also recognise that UC affects their ability to have children (17.2%) and their ability to care for them (41%).
As explained in one of the support platforms you are informed of when you are diagnosed with IBD, Educainflamatoria 1, it is important that upon diagnosis of the disease, we become aware of what our new condition means and that we rely on the team of professionals around us to manage the possible frustration, fear or uncertainty that may arise in any of these areas.
We must understand that when we do not ask questions, the problem does not exist for others and, therefore, it will not be addressed and solutions will not be provided.
It is essential to be able to confidently discuss these issues with the medical team supporting you, even though it is sometimes difficult to openly share aspects of your intimate life with health professionals, or you may not be clear about whether these issues should be discussed with them or with another professional, or whether they are not considered a priority in your health.
Nursing, within the multidisciplinary team that will work hand in hand with the patient, has a very important role in this area. One of their tasks is to provide emotional support and health education and to accompany the patient in this process.
If you feel that living with your disease is causing you stress, anxiety or sadness, speak to a professional you trust so that they can help you, both clinically and emotionally, to manage the impact that the symptoms are having on your life. They will also advise you or refer you to professional experts in employment issues.
With help, planning and care, it is possible to have a full life with less negative physical, psychological, social and sexual impact from your IBD.
- Marín-Jiménez, I., Gobbo Montoya, M., Panadero, A. et al (On behalf of GETECCU Study Group and ACCU): Management of the Psychological Impact of Inflammatory Bowel Disease: Perspective of Doctors and Patients—The ENMENTE Project, Inflammatory Bowel Diseases, Inflamm Bowel Dis, 2017, 23(9),1492-1498, Doi:10.1097/MIB.0000000000001205. https://academic.oup.com/ibdjournal/article/23/9/1492/4560710?login=false
- https://educainflamatoria.com/bienestar-y-apoyo-emocional/como-afecta-la-enfermedad-inflamatoria-intestinal-a-mi-bienestar-emocional-2/
- https://educainflamatoria.com/vida-sexual/
- Calvet X, Argüelles-Arias F, López-Sanromán A, Cea-Calvo L, Juliá B, Romero de Santos C, Carpio D. Patients’ perceptions of the impact of ulcerative colitis on social and professional life: results from the UC-LIFE survey of outpatient clinics in Spain. Patient Preference and Adherence. 2018:12 1815–1823.
News
The role of nursing staff in IBD
September 13, 2024
Patient

Inflammatory bowel disease (IBD) is chronic in nature. This means that the disease evolves over time in different ways and it is necessary to support the patient on an ongoing basis, since living with it often has a high impact on the quality of life of the patients and their families, affecting them not only physically, but in all areas of their lives: their social lives, families, relationships, work, school and emotional state. This circumstance requires specialised health professionals: medical teams, psychological care and nursing professionals.
Some more frequent symptoms, such as pain, fatigue, tiredness, body image disorders, or inflammation, can affect mood and generate high levels of stress, anxiety and an increased risk of depression. All of this can lead to abandonment of treatments, an increase in outbreaks and, as a result, poor control of the disease, making an interdisciplinary and multidisciplinary approach essential.
The appearance of symptoms, sometimes non-specific, throughout the course of the disease requires fluid communication between the different care centres and easy access to both the medical and nursing teams so that the patient can receive care adapted to their physical, emotional and professional needs.
For this reason, it is common to find a specialised team, trained and up-to-date on inflammatory bowel disease, in referral centres. In addition, in order to meet these needs, the N-ECCO (Nurses-European Crohn’s & Colitis Organisation) was created at european level to standardise criteria and share experiences that enrich the work carried out by these professionals when accompanying patients with IBD, so that this work is as optimal as possible and adapted to their individual and specific needs.
How does a nurse help a patient with IBD?
The bond that is created between the medical team and patients suffering from a chronic disease is very close. They all work hand in hand so that the patient understands and accepts their disease as soon as possible after diagnosis in order to integrate it into their daily life, taking into account each person’s specific needs.
This is why the nursing team performs vital work in order to design a specific care plan for each patient. These include the following:
- Establishing the beginning of a trusting relationship with the patient.
- Providing the patient with quality information so they can understand the disease and its care, resolve any doubts they may have about it and introduce healthy habits into their life that improve their autonomy and control of the disease.
- They provide information on how to access the IBD Unit, explaining how visits to the IBD Unit are organised, when it is necessary to go there, what are the warning signs and symptoms of the disease and how to act in each case.
- Helping and supporting the patient in the acceptance of the disease: understanding the impact it will have on their life in the future, the potential limitations they may face and the changes they will need to introduce in their life at each stage of their disease.
- Detecting the need for emotional support during this period or at certain times throughout the disease so that their quality of life is affected as little as possible.
- Checking the patient’s immunisation status before starting any immunosuppressive treatment and scheduling, updating and administering the necessary vaccinations and recording their effectiveness.
- Involving and educating the patient on the importance of adherence to treatment as the best strategy for successful disease management and flare-up prevention.
- Administering some pharmacological medications or hospital therapies and carrying out and necessary session planning, test requests or coordination with other medical teams, as well as educating and informing the patient regarding pre- and post-treatment precautions, if necessary.
- As it is an immunological disease, it is possible that some extraintestinal manifestations may appear that require treatment or other types of follow-up by the nursing staff, as well as multidisciplinary management.
Situations that may require contact with a nurse
There are a wide variety of situations that may require consultation with nursing staff. We will highlight some of them below:
- Suspicion of worsening of the disease or presence of symptoms associated with the onset of an flare-up.
- Doubts regarding prescribed medical treatments (dosage, regimen, form of administration, side effects, interactions, etc.).
- Requesting scheduled follow-ups of the disease.
- Requesting information on pending diagnostic tests and the necessary preparations for such tests.
- Gathering information on topics related to the disease (symptoms, extraintestinal manifestations, diet, healthy lifestyle habits, exercise, consumption of toxins, sexual relations, pregnancy, breastfeeding, medications, vaccines, contraceptives, travel, etc.).
- Verifying the information about the disease obtained from different sources (internet, family, friends, etc.).
- Communicating the presence of changes and discomfort in the perianal area.
- Checking the appearance of extraintestinal manifestations of IBD (dermatological, ophthalmological, rheumatological and nephrological).
- Reporting a pregnancy or clarifying related doubts.
Role of the nursing team in patients undergoing surgery
When surgery is part of the treatment of IBD, the nurse has a very important role to play in resolving any possible doubts or problems that may arise regarding the management, handling and acceptance of the ostomy, if necessary. A nurse specialised in ostomy care, advice and/or counselling is called a stomal therapist.
The placement of an ostomy pouch can be a challenging experience for some patients, not only on a practical level but also on an emotional level. This procedure is performed through surgery, so for it to work successfully, close communication with the patient should be established both before and after surgery, informing the patient about the preoperative period and also seeking a space where they can express their concerns and doubts, not only physical, but also emotional, both for the acceptance of the ostomy, and so that, in the future, the effectiveness of this measure is not compromised, providing clear guidance on the care and maintenance of the ostomy.
In short, nurses are an essential part of the team of healthcare professionals who will accompany people suffering from IBD throughout the course of their disease. In addition, they will often be the direct and most common point of contact with the patient for the entire medical team, playing a key role in establishing and promoting good communication with the rest of the medical team.
- https://www.ecco-ibd.eu/about-ecco/ecco-operational-board/n-ecco.html
News
Fecal calprotectin (FC): What is it and what role does it play in Inflammatory Bowel Disease?
March 7, 2024
Patologies

In Inflammatory Bowel Disease1 there is an inflammation of the intestine that causes neutrophils to infiltrate to the inflamed area to act. In this inflamed environment, and to defend the body from the entry of bacteria from inside the intestine due to the disruption of the intestinal barrier and its increased permeability, neutrophils “commit suicide” in a process known as Netosis, forming NETs, structures with a network structure, whose function is to destroy the largest number of “intruding” bacteria as quickly as possible, so that they release all the intracellular contents to the outside. A very high percentage of neutrophil cytoplasm consists of calprotectin, which is a protein highly resistant to bacterial degradation and stable at room temperature for days. This calprotectin passes into the lumen of the intestine (since the intestinal barrier has lost its integrity) and is eliminated from the body through the feces, hence its name fecal calprotectin (FC). Thus, by measuring the levels of calprotectin in the stool, it is possible to determine, by its concentration, whether the patient is in an active flare or not, and even the severity of the disease.
The measurement of fecal calprotectin is very common in the diagnosis of IBD, to determine and evaluate the state of the disease. In addition, it is a biomarker that allows to analyze in a non-invasive way, the changes of a patient at the intestinal level over a long period of time.
How is a fecal calprotectin test performed and when is the best time to perform it?
Since the measurement of this protein is performed through the stool, it will be necessary to take a stool sample from the patient and analyze it. GETECCU’s recommendations for sample collection2 are as follows:
It is recommended to collect a small amount of stool (approximately 3-5g) and deposit it in a collection container that is usually dispensed at the requesting center. This container does not require any specific treatment. The sample can be taken from any part of the stool, as it has been shown that CF is distributed homogeneously3 and at any time during the course of the disease.
As a precaution and to obtain a reliable result, a marked decrease in FC levels has been observed during preparation for colonoscopy4. Therefore, in case the patient is scheduled for one, caution should be taken to collect the sample before starting the colonic cleansing or several days after the test.
What does it mean when fecal calprotectin is elevated?
When CF is elevated in inflammatory bowel disease, it means that there is inflammation in the bowel. As a rule, high levels indicate bacterial infections, parasitic infections, colorectal cancer, or certain diseases that cause inflammation of the bowel, such as ulcerative colitis5 (UC) and Crohn’s disease6 (CD).
In both UC and CD this could mean that the disease is active and may be causing symptoms such as abdominal pain, diarrhea or bleeding as the immune system is fighting to decrease such inflammation in the gut.
Now that you understand what fecal calprotectin is, the most important thing is to trust your doctor, follow the prescribed treatment and communicate your symptoms so that he/she can plan the best strategy for managing your disease and perform the necessary tests at any given time.
- Ulcerative colitis and Crohn similarities – Adacyte
- Recomendaciones del Grupo Español de Trabajo en Enfermedad de Crohn y Colitis Ulcerosa (GETECCU) sobre la utilidad de la determinación de calprotectina fecal en la enfermedad inflamatoria intestinal | Gastroenterología y Hepatología (elsevier.es)
- Intra-Individual Variability of Faecal Calprotectin: A Prospective Study In Patients With Active Ulcerative Colitis | Journal of Crohn’s and Colitis | Oxford Academic (oup.com)
- Colonoscopy and ileoscopy: essential tests for diagnosing IBD – Adacyte
- What is ulcerative colitis? – Adacyte
- Ulcerative colitis and Crohn similarities – Adacyte
News
Colonoscopy and ileoscopy: essential tests for diagnosing IBD
May 5, 2023
Patient

Diarrhoea, abdominal pain, blood in stool, anaemia, fatigue, fever, weight loss. These are signs that can signal a digestive problem. As soon as it is suspected that a patient might have an inflammatory bowel disease (IBD), such as ulcerative colitis or Crohn’s disease, the healthcare professional needs reliable diagnostic tools to confirm these conditions, ruling out other types of diseases with similar symptomatology.
In addition to analytical tests on both blood and stool and radiological tests, endoscopic tests are a fundamental and invaluable technique for diagnosing IBD.
Enteroscopy, endoanal ultrasound, capsule endoscopy, upper gastrointestinal endoscopy or gastroscopy, and lower gastrointestinal endoscopy or ileocolonoscopy are included within these endoscopic tests. We will explain what this last technique, which includes colonoscopy and ileoscopy, consists of.
Ileocolonoscopy as a diagnostic tool
Ileocolonoscopy is one of the most common endoscopic tests performed to diagnose IBD. Thanks to it, healthcare professionals can view the intestinal mucosa directly, both the colon (colonoscopy) and the end of the small intestine or terminal ileum (ileoscopy).
Thus, it is possible to know whether a patient has Crohn’s disease or ulcerative colitis as the endoscopic features are singular and different to one another. Furthermore, it helps to choose the more suitable therapeutic option and surgical procedure, if necessary. The point is that the extent and severity of the damage, as well as its exact location in the colon and terminal ileum, can be visualised.. In the case of Crohn’s disease, it is normal for the ileum to be affected, hence the appropriateness of performing an ileoscopy alongside a colonoscopy in these cases.
On the other hand, these techniques are effective tools for ruling out drug-induced diseases, like anti-inflammatory drugs, or other types of conditions with similar symptoms, such as infectious colitis. Moreover, it is possible to take a biopsy (tissue samples) during the test, where necessary, to perform an anatomical-pathological examination or therapeutic procedures. This is the case of polypectomy (removal of polyps) or dilation of strictures (reduction of internal diameter of the intestine).
Long-term monitoring of a patient with IBD
Performing a long-term follow-up of the inflammatory disease’s progression is fundamental to anticipate flare-ups, assess the efficacy of the treatment and modify it if necessary. In this case, ileocolonoscopy is very useful as the extension and evolution of the condition can be viewed in the colon and the end of the small intestine or terminal ileum.
Patients with long-standing IBD are more likely to develop colorectal cancer than the general population. This risk that is higher or lower depending on the duration and extension of the disease. For this reason, endoscopic monitoring via ileocolonoscopy can be an effective tool for detecting pre-malignant lesions and acting as soon as possible, thus reducing the mortality rate associated with colorectal cancer. Another situation where it is very useful to perform an ileocolonscopy is after surgery. In fact, it is considered the ‘gold standard’ as it allows to establish the onset of morphological recurrence and its severity, which is directly related to the long-term clinical course1.
How should the patient prepare for the test?
Like any endoscopic procedure, both colonoscopy and ileoscopy require the patient to undergo pre-test preparation. These preparations include a special diet and, occasionally, the withdrawal of some of the drugs they are taking. In this latter case, the healthcare professional will inform you how to proceed with these drugs in order to avoid complications that may hinder the examination.
As for the diet2 that the patient should follow before the test, two days before it, he/she should start a low-residue diet. This means that fatty cheeses, full-fat dairy products, oily fish, fatty meats, cold meats, wholemeal products, fruits, vegetables, legumes, chocolate, pastries and dried fruit are forbidden.
On the other hand, the foods that can be eaten during the special diet are: skimmed milk and natural yoghurt, fresh cheeses, hard cheeses and a bit of butter; white bread or non-wholemeal toast and biscuits; soups without vegetables; non-wholemeal rice and pastas; skinless mashed or boiled potatoes; grilled or cooked white meat and fish; skinless quince, peaches in syrup, cooked or roasted apples or pears; tea, coffee or light infusions.
Colon cleansing will be started the day before the colonoscopy or ileoscopy, with preparations given by the medical professional. These can be polyethylene glycol solutions, magnesium salts, sodium phosphate solutions or enemas. However, the patient must stop eating solid foods 3 or 4 hours before starting the colon cleanse.From then on, they can only have clear liquids, in other words, water, infusions, filtered soups, coffee or tea, strained fruits juices and clear soft drinks. On the day of the test, the patient must stop drinking clear liquids 3-4 hours before the colonoscopy or ileoscopy is performed.
During and after the ileocolonoscopy
The test is performed in the Endoscopy Unit of the Gastroenterology Department. The test is carried out by Digestive specialist doctors with training in diagnostic and therapeutic endoscopy from the IBD Unit itself or, failing that, with IBD training.
Nursing staff specialised in endoscopy and nursing assistants also participate. Their function during ileocolonoscopy is to care for and look after the patient, help the endoscopist perform the test and administer the necessary medication.
Regarding the duration of the test, it can range from 20 to 60 minutes. It depends on the amount of intestine to be examined and, if it is necessary to perform any therapeutic procedure during the test. Moreover, sedation and intravenous analgesics are often administered to avoid discomfort for the patient and to perform the test without any pain.
After completing the examination, the patient is taken to another room where they will awaken with a feeling of abdominal bloating and discomfort that is similar to intestinal colic. This is due to the insufflated air inside the intestine during the examination. This discomfort will disappear after a few hours.
News
What are the most prevalent ocular extraintestinal manifestations linked to IBD?
March 16, 2023
Patologies
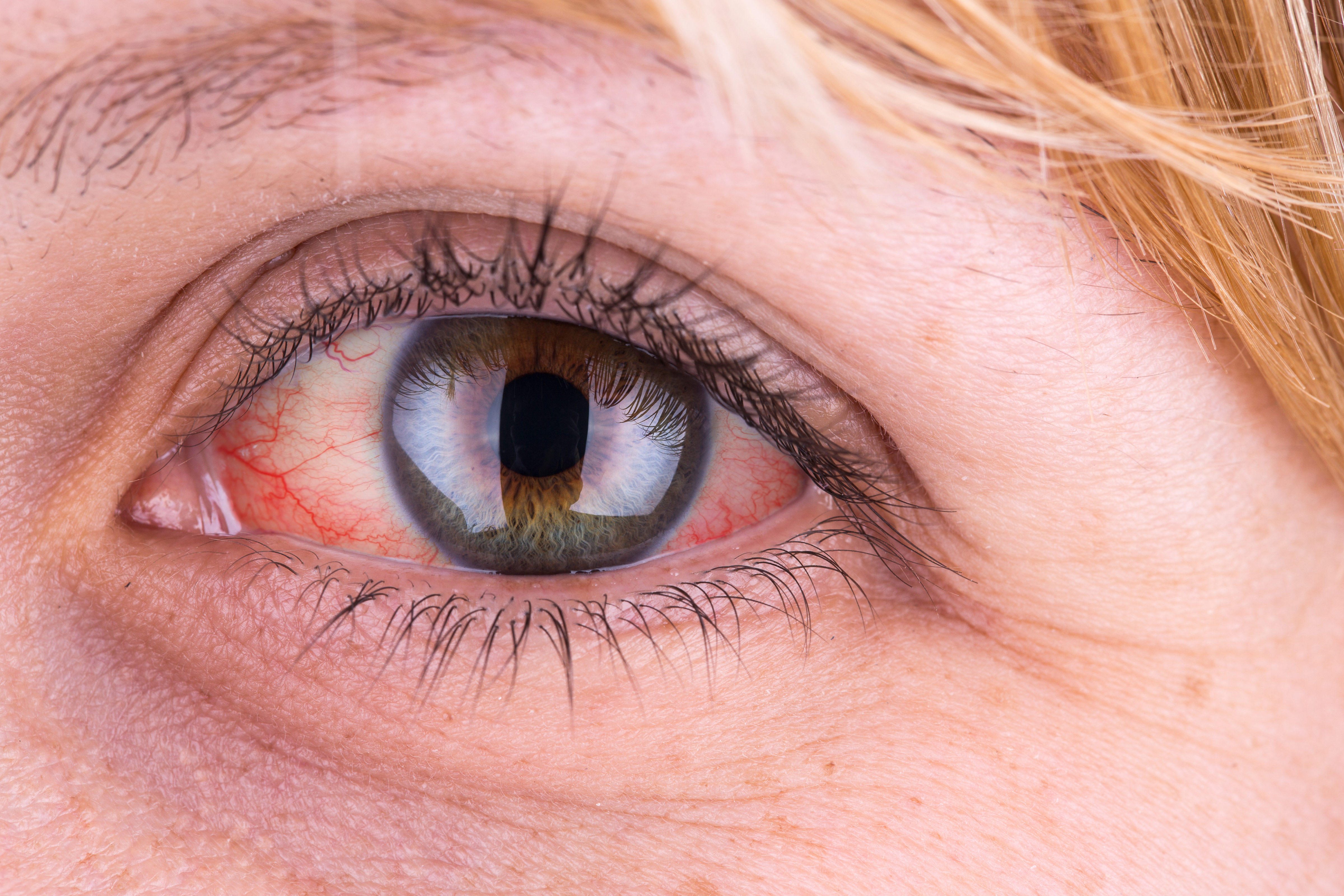
Inflammatory bowel disease (IBD) is considered a systemic inflammatory disease. In other words, in addition to intestinal damage, conditions may also develop in other organs and systems, like the eyes. They are known as extraintestinal manifestations (EIM), diseases that do not need to be closely linked to inflammatory activity in the intestine, despite occurring simultaneously. In fact, their triggering mechanisms are not precisely known, although it is believed that the cause can be linked to the interaction of genetic and environmental factors and changes in the gut microbiota. Ocular extraintestinal manifestations are not common in patients with IBD, affecting only 10%1. The consequence of this low prevalence is that both medical professionals and patients themselves overlook the possibility that symptoms like pain or eye redness are symptomatology linked to ulcerative colitis2 or Crohn’s disease. A mistake that can have serious consequences for patients that can be avoided with a multidisciplinary approach, including a complete ophthalmological examination.
The most common ocular alterations in patients with IBD are scleritis, episcleritis and uveitis. In the first two cases, the affected eye structure is the sclera, known as the white part of the eye; and in uveitis, damage is found in the uvea, the layer located below the sclera. It must be emphasised that onset of the three conditions often coincides with other skin and joint manifestations, which may provide a lead to the early detection of eye conditions.
Symptoms and treatment of episcleritis and scleritis
Episcleritis and scleritis are ocular extraintestinal manifestations that affect the white part of the eye, although each of them do so at different degrees.
Episcleritis occurs when the thin tissue layer covering the white part of the eye (episclera) is inflamed and irritated. An inflammation that often coincides with a flare-up of the disease. Its symptomatology is emphasised by a burning sensation in the eye that does not worsen on palpation, redness, watering and mild pain or discomfort.
Episcleritis treatment depends on the severity of the symptoms. The condition normally resolves with IBD treatment, even though it is sometimes combined with non-steroidal anti-inflammatory eye drops to relieve discomfort.
If episcleritis is not treated correctly on time, it is likely to develop into scleritis, a more severe eye issue that can result in vision loss. The symptoms of scleritis are severe eye pain that worsens on palpation and radiates to the forehead, cheek or paranasal sinuses; and more eye redness than during episcleritis.
In addition to ulcerative colitis and Crohn’s disease treatment, systemic corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs) or immunosuppressants, like methotrexate, are prescribed to treat and control scleritis.
How to detect uveitis
Uveitis is another ocular extraintestinal manifestation that is more common in patients with IBD. It often appears during both remission periods and flare-ups, or even before diagnosis of the inflammatory disease. It is characterised by inflammation of the layer located below the white part of the eye, the uvea, where a large amount of blood vessels are found.
When inflammation occurs in the frontal part of the eye, it is called anterior uveitis. It is the most common form of uveitis and its symptoms are eye redness, sensitivity to light (photophobia), eye pain, watering and blurred vision. If this symptomatology is combined with reduced vision and/or appearance of floaters, the patient may suffer from posterior uveitis.
If they experience one of the symptoms described above, they should visit their doctor as soon as possible because the consequences can be serious, even leading to permanent vision loss. The symptomatology can either occur suddenly and worsen at short notice, or they may begin gradually. It is therefore an ophthalmological emergency and an early diagnosis is necessary to avoid complications.
Uveitis treatment involves the application of cycloplegic eye drops to relieve the pain and avoid posterior ocular adhesions. Topical, ocular, periocular or systemic corticosteroids and even immunosuppressants are often used in the most severe cases.
News
Planning a pregnancy in women with IBD
February 6, 2023
Patient

When deciding to have children, questions regarding planning, the pregnancy itself, the delivery or breastfeeding, lie ahead. Even though it arrives with much hope and anticipation, it is a new phase in life that is not without fear and uncertainty. Perhaps one of the main fears for future mothers and fathers is the possibility that the baby is born with some type of condition that may affect its quality of life.
Hence the importance of planning a pregnancy, especially when we are talking about patients with inflammatory bowel disease (IBD), such as ulcerative colitis or Crohn’s disease. Although the majority of pregnancies in patients with IBD are successful and have no complications, it is essential to seek a consultation with healthcare professionals prior to conception to assess the patient’s condition, when it is advisable for her to become pregnant or what the risk factors are, as well as to explain what vitamin complexes she needs during pregnancy.
In this article we will explain in detail the aspects to be taken into account by IBD patients, mainly women, when they wish to have children.
First step: planning a pregnancy
Couples where at least one of the two parents has IBD must plan a pregnancy in advance in order to establish specific care and tests, for both the mother and the foetus. Some of these tests verify that the patient has no vitamin B12, iron and folic acid deficiencies, or macro- and micronutrient deficiencies among others. In addition to such an important point, it is necessary to identify whether the patient has dysplasia (growth of abnormal cells within a tissue or organ) or uterine cervical and colon carcinomas as these will directly affect their pregnancy.
On the other hand, it must be emphasised that the greatest risk for mother and foetus, perhaps above other factors, is active IBD. Therefore, the patient must never stop treatment on their own accord. Neither before nor during pregnancy, as they could have a relapse. The majority of complicated pregnancies (premature birth, low birth rate) are linked to the inflammatory process itself. Hence why it is a key aspect.
To ensure that the pregnancy runs as smoothly as possible and to avoid risks, the responsibility for caring and management of pregnant women falls to a multidisciplinary team of gastroenterologists and IBD surgeons, as well as obstetricians with expertise in high-risk pregnancies and paediatricians experts in newborns born from IBD parents.
Fertility: Active IBD vs inactive IBD
The majority of studies performed on fertility in men and women with IBD show that fertility is not affected when the disease is inactive. In fact, they are as fertile as the general population. Moreover, a complication-free pregnancy is possible as long as the disease is not active.
Nevertheless, it is common that fear of adverse drug reactions on the foetus, of having a flare-up during pregnancy or of not being able to combine the disease with children, leads patients to make the decision not to have children. Hence, the fact that the number of pregnancies in patients with ulcerative colitis or Crohn’s disease is lower than in the general population is mainly due to a carefully considered decision taken within each couple rather than to infertility per se.
Another reason why patients with inactive IBD voluntarily decide not to become parents is the idea that the baby may develop their disease, which is also an obstacle. In this respect, if only one parent has IBD, the chance of the child developing the disease is less than 5.2%. This percentage increases to 33% if both parents have some form of inflammatory bowel disease1.
On the opposite side are the patients with active IBD, whose fertility can be affected. Sometimes the outbreak itself or being in a situation of malnutrition can be the factors that reduce fertility, although they are not the only ones. Other mechanisms that can influence it are: inflammation spreading to the Fallopian tubes and ovaries in Crohn’s disease, when intercourse is painful (dyspareunia) due to active perianal disease or when adhesions have formed in the pelvis after surgeries like proctocolectomy with ileoanal pouch.
Despite this dark scenario, there are studies offering hope to patients undergoing proctocolectomy with ileoanal pouch who have problems conceiving. In these cases, in vitro fertilisation techniques are a possibility for them to consider because pregnancy rates are similar to those of patients with ulcerative colitis, with or without an ileoanal pouch2.
Under no circumstances must patients stop treatment when they become pregnant without first consulting their medical professional. Why? Because stopping or suspending medication on their own decision is worse and more harmful than the treatment’s possible adverse events.
Even though the majority of drugs are currently considered safe during pregnancy and breastfeeding, the following are unsuitable for pregnancy: Methotrexate, Tofacitinib, Thalidomide, 6-Thioguanine (pregnancy) and Ciclosporin (breastfeeding). For men, sulfasalazine treatment can affect sperm count and motility, although it is reversible.
To avoid reaching this situation in which the patient is taking drugs that are contraindicated for pregnancy or can abandon the treatment on his/her own, the healthcare professional must know, as explained above, the patient’s intention to have children, because only then can he/she replace the treatment with other drugs or techniques such as granulocyte-monocyte apheresis, more suitable for pregnancy.
This latter procedure, granulocyte-monocyte apheresis, is a non-pharmacological treatment that involves removing inflammatory cell lineages or mediators from the bloodstream by passing the blood through a column filled with cellulose acetate beads where these are adsorbed/retained. This process is a non-pharmacological treatment that offers an effective and safe alternative to patients who do not respond to other treatments or, as in the case of pregnant women, cannot take certain drugs due to the side effects they cause.
- FERTILIDAD Y EMBARAZO EN PACIENTES CON ENFERMEDADES INFLAMATORIAS INTESTINALES | Revista Médica Clínica Las Condes (elsevier.es)
- In Vitro Fertilization Is Successful in Women With Ulcerative Colitis and Ileal Pouch Anal Anastomosis – PubMed (nih.gov)
- FERTILIDAD Y EMBARAZO EN PACIENTES CON ENFERMEDADES INFLAMATORIAS INTESTINALES | Revista Médica Clínica Las Condes (elsevier.es)
News
Granulocyte-monocyte apheresis in patients with ulcerative colitis
January 10, 2023
Adacolumn

After having been diagnosed with ulcerative colitis (UC) or Crohn’s disease, the path patients with inflammatory bowel disease (IBD) and their families take is hard. Accepting the news they have received, attending all the consultations with specialists, performing the relevant tests to understand the scale of the disease or the time it takes to adjust and establish the correct treatment, are just some of the obstacles and challenges they must overcome. Indeed, one of the most complex points that the patient has to face is to succeed in receiving appropriate treatment.
Focusing on the case of ulcerative colitis, a condition that causes inflammation in the rectum and the colon, the patient suffers relapses with more or less intense activity flare-ups, which are more or less long-lasting. The current drugs in the healthcare professional’s therapeutic arsenal for treating patients aim to induce remission of these flare-ups and keep IBD inactive to improve the patient’s quality of life. With the best efficacy and safety possible, of course.
Taking into account that some patients do not respond to conventional treatments or cannot use them due to their profile, healthcare professionals have seen granulocyte-monocyte apheresis (GMA) as a therapeutic ally offering proven benefits in patients with ulcerative colitis. This happens because the technique reduces the amount of existing inflammatory cells in the bloodstream without giving the patient anything.
What is granulocyte-monocyte apheresis?
As commented above, GMA is a non-pharmacological treatment whose basis is to pass the patient’s blood via an extracorporeal device to remove from it those pathogenic inflammatory components that determine or perpetuate the disease, thereby contributing to their treatment.
One of the granulocyte-monocyte apheresis systems sold in Europe is a system comprising a column or filter with cellulose acetate beads that enable the selective adsorption of 65% of granulocytes, 55% of monocytes/macrophages and 2% of lymphocytes, removing them from the bloodstream.
The procedure involves taking blood from the patient’s cubital vein, which flows through the circuit and the adsorption column where it is purified, and is re-infused via the contralateral cubital vein (fig. 1, we include the image of the process).
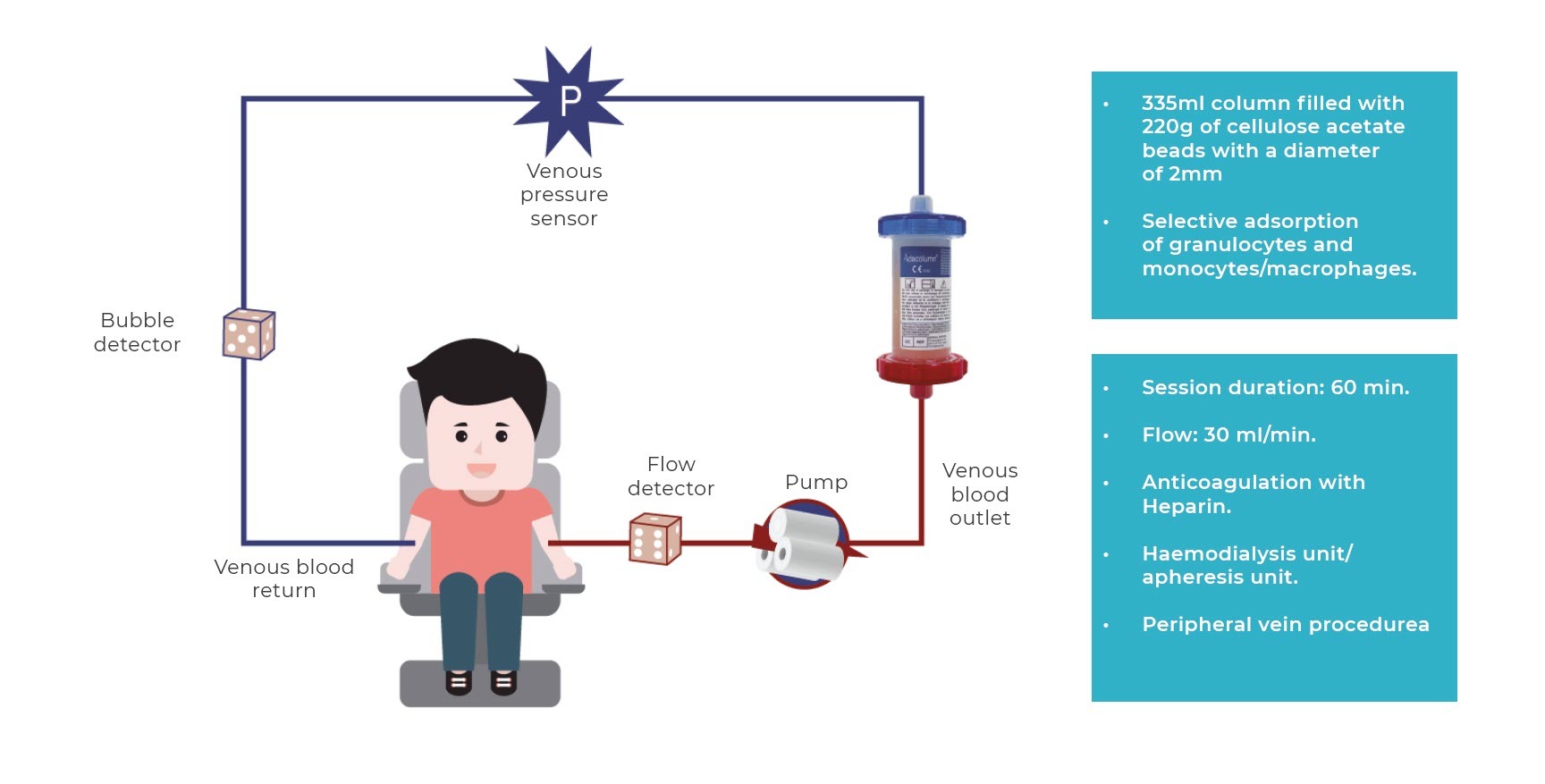
The procedure is performed in haemodialysis or apheresis units, although it can be performed in treatment units at day clinics after suitable training. The regimen for applying the technique (frequency and number of sessions) ranges from 5 to 10 sessions (1 or 2 a week) of 60 minutes or more, although actual clinical practice in the majority of hospitals involve an induction of 10 sessions (2 sessions/week for the first 3 weeks to accelerate response and then 1 weekly session until completing 10) and for a longer duration (normally 90 minutes), as this regimen has been observed to be safe and well-tolerated, obtaining the best clinical results.
Nevertheless, the only practical limitation to performing it is poor accessibility for inserting peripheral lines, which may require inserting a central line.
GMA’s mechanism of action is currently still not completely known. However, it is known that peripheral blood granulocytes and monocytes/macrophages are elevated and activated in many autoimmune diseases, whose numbers are linked to the activity and severity of the disease, and which play a key role in the disease immunopathogenesis while producing larger amounts of pro-inflammatory cytokines that are responsible for the tissue damage.
It is believed that GMA’s main adsorption mechanism is linked to the activation of the complement system’s cascade and the induction of granulocyte adhesion to the column.
Leukocytes that express Fc gamma receptor (FcγR) and complement receptors (Mac-1, CD11B/CD18) adhere to the cellulose acetate beads through activation of the complement. Thus, the decreased reservoir of activated granulocytes in the circulatory system is compensated by the mobilisation of young inactive granulocytes (CD10-) from the bone marrow to the bloodstream, without the ability to migrate to the inflammatory focal point.
Likewise, a functional change occurs in the activated monocytes, which express CD14+CD16 markers, which altogether leads to a reduction in the production of pro-inflammatory cytokines and an increase in circulating anti-inflammatory mediators; in summary, a phenomenon of immunomodulation and, accordingly, a reduction in inflammatory infiltrate and tissue damage. The direct consequence of removing leukocytes from the circulatory system is the mobilisation of young inactive leukocytes from the bone marrow, which cannot migrate to the inflammatory focal point. What is more, passing the blood through the column, in addition to decreasing the total number of inflammatory cells in the blood, also causes changes onto the surface of those that return to the body leading to a series of immunological changes that enhance the activation of previously inhibited anti-inflammatory mechanisms, initiating the resolution of inflammation. By doing so, in addition to producing immunomodulation (a change in the immune system), it reduces inflammation and tissue (cell) damage in the intestinal mucosa.
GMA is indicated for use in which patients?
There is currently a very broad therapeutic arsenal for treating IBD even though for a number of patients, these medications are ineffective or have adverse events2. Other therapeutic options are therefore needed to monitor the progression of the disease and avoid surgical procedures.
In certain scenarios, GMA is an alternative for treating this disease. This technique can be applied to different situations, including patients that do not respond well to conventional pharmacological treatments, or have a corticosteroid-dependent course, preventing relapse and in whom immunosuppressive or biological treatment is considered3,4.
Despite seeking the best treatment for each case, there is a high percentage of patients with ulcerative colitis that do not respond to conventional treatments,either those based on corticosteroids or immunomodulators (IMM thiopurines) (Ardizzone et al, 2006) or anti-TNF therapy. Until a few years ago, when a healthcare professional was in this situation where drugs failed to improve the patient’s condition, the most used option for treating them and improving their quality of life was surgery.
However, in recent decades, other treatment alternatives for patients with ulcerative colitis have emerged, like GMA, which are safer and can be applied to the following patients1:
- Adult patients with corticosteroid-dependent ulcerative colitis after failure, intolerance or elevated risk of immunomodulatory treatments and/or biologics2.
- Elderly patients with comorbidities.
- Pregnant patients.
- Paediatric patients with ulcerative colitis.
The contraindications are:
- Granulocyte levels below 2000/ML
The warnings are:
- Heparin allergy and heparin-induced thrombocytopenia
- Severe anaemia (Hb < 8 g/dL)
- Severe coagulopathy
- Active infection
- Severe heart or kidney disease
- Precautions:
- Care in situations of hypercoagulability (fibrinogen > 700 mg.mL) or dehydration (diarrhoea or recent fevers). These factors need to be corrected beforehand.
GMA, significance of efficacy and safety in UC treatment
If there are two features that define GMA, they are its safety and efficacy. As stated by Prodiggest Project3, this therapeutic option has been the subject of studies andmeta-analysis that describe it as an effective and safe alternative for patients.
On the one hand, GMA is described as being very safe for patients with ulcerative colitis because the adverse events of conventional treatments disappear. In this case, the majority of side effects are mild and temporary allowing the patient to continue with the treatment. Notably among them are headaches, chills, low-grade fever, dizziness, fatigue, myalgia, palpitations, hypotension or redness. In many case, the adverse events are linked more to the apheresis technique than to GMA treatment itself (issues with the lines etc), hence the importance of being performed by skilled professionals.
On the other hand, in addition to its efficacy in paediatric, pregnant or elderly patients, or corticosteroid-dependent and corticosteroid-refractory patients, there are other scenarios where GMA is effective. For example, it has proven that it can be a first-line treatment in distal ulcerative colitis with mild-moderate activity with a remission induction rate of 70% (Yamamoto et al 2004) and up to 80% in patients whose disease is less developed, steroid-naive (Takemoto et al 2007), as stated in Prodiggest Project.
Furthermore, it is an option that can prevent relapse in certain patients at high risk of having recurrent and difficult to control flare-ups. Accordingly, a mean duration of clinical remission obtained with GMA of 10 months can be established in patients with ulcerative colitis (Ljung et al 2007), and can even be much longer than a year the earlier the disease or the less treatment the patient has received prior to GMA (corticoids, thiopurines, biologics, etc.).
- https://www.aegastro.es/publicaciones/publicaciones-aeg/protocolos-asistenciasles-prodiggest/uso-racional-de-la-granulocitomonoaferesis-en-la-enfermedad-inflamatoria-intestinal
- Adacolumn® – Adacyte
- https://www.aegastro.es/publicaciones/publicaciones-aeg/protocolos-asistenciasles-prodiggest/uso-racional-de-la-granulocitomonoaferesis-en-la-enfermedad-inflamatoria-intestinal
- Dignass A, Lindsay JO, Sturm A, Windsor A, Colombel JF, AllezM, et al. Second European evidence-based consensus on thediagnosis and management of ulcerative colitis part 2: Currentmanagement. J Crohns Colitis. 2012;6:991—1030.
- Dignass A, Akbar A, Hart A, et al. Safety and efficacy of granulocyte/monocyte apheresis in steroid-dependent active ulcerative colitis with insufficient response or intolerance to immunosuppressants and/or biologics [the ART trial]: 12-week interim results. J Crohns Colitis. 2016;10:812–820.
- Dittrich K, Richter M, Rascher W, et al. Leukocytapheresis in a girl with severe ulcerative colitis refractory to corticosteroids, infliximab, and cyclosporine A. Inflamm Bowel Dis. 2008;14:1466–1467.
News
Inflammatory bowel disease in elderly patients
December 13, 2022
Patient

Monitoring nutrition and staying physically active are the two key points for leading a healthy lifestyle. Although this fact is important at any age, it is even more so if we wish to reach old age in good health conditions. The onset of conditions, such as inflammatory bowel disease (IBD), is possible during this phase, especially from the age of 60. Out of the elderly patients diagnosed with ulcerative colitis1 or Crohn’s disease for the first time, 65% are aged between 60 and 69 years; 25% between 70 and 79 years; and 10% over the age of 80.2
Inflammatory bowel diseases are often accompanied by another type of known secondary condition, such as extraintestinal manifestations (EIM), which affects the skin, eyes or joints, even though they are less common in elderly patients. There are also surgical procedures, postoperative recurrence and the onset of more aggressive or severe forms of IBD.
Malnutrition, anaemia and osteoporosis in elderly patients with IBD
Having a varied, complete, balanced diet3 in elderly patients, especially those with IBD, is fundamental but not always feasible. Issues can arise whilst chewing and swallowing due to tooth loss and decreased salivation, or can worsen the digestive process as a consequence of the reduced amount and quality of digestive secretions that, accompanied by intestinal mucosal atrophy, results in worse absorption and reduced benefit from some nutrients, mainly proteins, vitamins and minerals.
The issue of malnutrition thereforearises due to a declining diet, which causes anaemia4. Although this is not the only reason. Elderly patients with IBD can also have anaemia and malnutrition due to blood loss via the gastrointestinal tract. Hence the need for elderly patients with ulcerative colitis and Crohn’s disease to ensure they are ingesting iron-rich foods daily, notably fish, meat and eggs.
Malnutrition in elderly patients with IBD is also one of the causes for the onset of osteoporosis. Calcium, phosphorus, magnesium and vitamin D deficiencies, among other components required for bone formation, influence the loss of bone mineral density and bone weakening or fragility, thereby increasing the risk of fractures.
To prevent osteoporosis in patients over the age of 60, it is recommended to stop smoking, take the right amount of calcium and vitamin D, and exercise regularly. In fact, moderate physical activity increases bone mass and strengthens muscle. Dancing, walking, running, performing aerobic exercise, climbing stairs or lifting weights are some of the activities that the population at risk of osteoporosis should perform.
Treatment of elderly patients with IBD
The healthcare professionals’ criteria for selecting a treatment and establishing the regimen to be followed by elderly patients with ulcerative colitis or Crohn’s disease are often similar to those taken into account when determining medication for any other population group. Even the efficacy and results that can be expected from the drugs are also similar.
Nevertheless, when patients over the age of 60 have comorbidities, it is possible that the impact of adverse drug reactions are greater. In these cases, consultant specialists count on their therapeutic arsenal with treatment options, such as granulocyte-monocyte apheresis (GMA)5. Thanks to this non-pharmacological treatment, activated leukocytes that are responsible for intestinal inflammation are safely removed from the patient’s blood. In this way, safety is increased and risks to fragile patients, such as elderly patients, are reduced to a minimum.
News
Surgery for ulcerative colitis: before, during and after
November 8, 2022
Patient

Physicians have an extensive therapeutic arsenal for treating patients with ulcerative colitis. Available drugs keep the disease inactive or in remission in most cases. Despite this between 25% and 40% of patients with ulcerative colitis will need surgical treatment at some point in their illness1.
Unlike Crohn’s Disease2, surgery in ulcerative colitis is curative. The fact is that, by affecting the rectum and the colon, its removal implies the total healing of the patient.
In particular, surgery is indicated3 when the pharmacological treatment has not controlled the symptoms of ulcerative colitis; when complications such as stenosis (narrowing or reduction of the internal diameter of the intestine), perforation, severe bleeding, abscesses or fistulization occur; when premalignant or carcinogenic lesions develop; or when perianal disease occurs and drainage surgery is necessary, derivative colostomies to isolate fistulas from passing stool or radical protections in advanced cases.
Preparation of the patient before surgery
The surgeon and the gastroenterologist study the progress of ulcerative colitis in the patient to determine the extent and severity of the symptoms. Afterwards, they inform him about the technique best suited to his situation and the benefits, complications and risks associated with it4.
Before surgery5, the patient will undergo a preoperative study consisting of: blood and urine analysis, chest x-ray and electrocardiogram. In addition, it is very important for the patient to be in good general condition and to discontinue the treatment he is taking (corticosteroids, immunosuppressants or biologic therapy, granulocyte apheresis…), if any.
Two days before the intervention, the patient should follow a liquid diet so, with the help of an intestinal preparation, the intestine is emptied of waste or traces of feces.
Surgical interventions in the treatment of ulcerative colitis
The gastroenterologist and surgeon may choose from a variety of surgical techniques to treat ulcerative colitis6. Among the most common ones stand out: the total proctocolectomy with ileostomy or with ileoanal reservoir. It is also very common to perform a total colectomy with ileorectal anastomosis, and subtotal colectomy with ileostomy and rectosgmoid mucous fistula.
When a total proctocolectomy is performed, the entire rectum and colon are resected. If it is decided to perform a total proctocolectomy with ileostomy, an opening or hole is made that connects the ileum to the outside (ileostomy) to remove the intestinal waste in a bag (ostomy).
In the event that medical professionals choose to perform a restorative proctocolectomy or ileoanal reservoir, an internal reservoir or pouch is created with part of the small intestine (ileum) that will be attached to the anus and function as a new rectum.
The technique known as total colectomy with ileorectal anastomosis consists in resecting the entire colon and joining (anastomosis) the ileum with the rectum. For its part, in the subtotal colectomy with ileostomy and rectosgmoid mucous fistula, only the affected areas of the colon are resected and an ileostomy is performed. If the sigma (the end of the colon) is not affected, it is left intact and communicates with the outside through the anus or through a mucous fistula performed on the abdominal wall for the secretions to come out.
What happens after surgery in ulcerative colitis?
After the surgery in ulcerative colitis, the patient’s recovery comes. Initially, he will not be able to ingest any type of food. He will only receive nutrients through parenteral nutrition, intravenously. Once the intestinal movement is restored, he can gradually begin to swallow liquids and subsequently solids.
Furthermore, it is common for the patient to evacuate traces of blood, mucus and/or feces through the rectum, sometimes, without being able to help it. That is called rectal incontinence. If the rectum is intact, he will not experience any pain during evacuation. The frequency of these secretions will decrease over time.
In the case of an ostomy, the patient should begin to get used to his new situation as soon as possible. His intestinal function will be altered, his body image will change and he will have a stoma. During his hospital stay, healthcare professionals will help the patient and his family adapt, offering them all the advice and information they need.
However, given the changes in the patient’s quality of life and the complications usually associated after this surgery (cross with new article commenting on this topic), it is always reserved as the last alternative and when the rest of available treatments have not been effective in the control of ulcerative colitis.
- https://www.elsevier.es/es-revista-cirugia-espanola-36-articulo-estado-actual-del-tratamiento-quirurgico-S0009739X12003119
- Ulcerative colitis and Crohn similarities – Adacyte
- https://www.elsevier.es/es-revista-cirugia-espanola-36-articulo-estado-actual-del-tratamiento-quirurgico-S0009739X12003119
- https://www.educainflamatoria.com/que-preparacion-previa-tiene-una-cirugia-de-eii
- https://www.elsevier.es/es-revista-enfermedad-inflamatoria-intestinal-al-dia-220-articulo-manejo-perioperatorio-enfermedad-inflamatoria-intestinal-S1696780115000767
- What is ulcerative colitis? – Adacyte
News
Biologic treatment for Ulcerative Colitis: a therapeutic revolution
October 13, 2022
Patologies

The last 30 years have been a revolution in the treatment of Inflammatory Bowel Disease (IBD). Healthcare professionals have incorporated into their therapeutic arsenal new molecules that have been shown to be highly effective in Crohn’s Disease and Ulcerative Colitis. In addition, these molecules have made it possible to expand the therapeutic options available to the patient and to move towards Personalized Medicine. We are talking about monoclonal antibodies.
These new drugs are based on different mechanisms of action to which we are accustomed. This is why they will allow, in the very near future, to manage the disease in a much more varied way. Experts predict that the greatest revolution in this field is yet to come. For the time being, they are getting an effective treatment for patients suffering from a moderate to severe outbreak and who have an unfavorable response to conventional treatments or are intolerant and/or have contraindications to such treatments.
What are the biological treatments for Ulcerative Colitis?
Monoclonal antibodies are a type of protein that binds to a cytokine (another type of protein) in the organism called Tumor Necrosis Factor alpha (TNF-alfa). Thus, biological treatment can block TNF activity. This cytokine is one of the molecules responsible for the inflammatory process when an outbreak occurs1 in patients with IBD such as Ulcerative Colitis.
We therefore refer to complex compounds synthesized from an organism or a living cell that are genetically modified with technology and genetic engineering, in other words, by means of an effective and precise biotechnology that allows the manipulation of those cells or microorganisms.
So it can be said that the biologic treatment of Ulcerative Colitis improves patients’ quality of life. That is, unlike other existing medicines, these new biologic drugs allow the disease to be kept in remission for longer periods. In this way, the patient can carry out his daily activities normally without presenting any symptoms.
When and how is administered a biologic drug?
Biologic drugs are indicated for both induction and remission of Ulcerative Colitis. Before recommending administration, the health care professional will focus on the patient’s vaccination status and his immunization status against some infections.
In addition, he will rule out a latent tuberculosis infection. If the patient were in this situation, the bacteria responsible for tuberculosis would be alive in his organism but inactive. Therefore, he would have no symptoms until the virus was activated. In order to rule out this possibility tests such as a chest x-ray, a blood test and a tuberculin test (mantoux) will be performed.
Afterwards, the physician will evaluate which biologic drug to administer the patient from the entire arsenal available. Then, the dose will be stablished and the most appropriate time to start the biologic treatment of Ulcerative Colitis with biologic drugs will be evaluated.
Two forms of administration may be used2 depending on the drug selected:
- Intravenous. The drug is administered at the hospital using a venous line. Administration will be slow to avoid a reaction to the medication. This is how infliximab, its biologic and vedolizumab are administered.
- Subcutaneous. The drug can be administered at home by the patient himself as if it were an insulin injection. Adalimumab and golimumab are administered using this method.
In the case of ustekinumab, the first dose is administered intravenously. Subsequent doses are administered subcutaneously.
Diversity of biologic treatments for Ulcerative Colitis
The approval of infliximab marked a turning point in the treatment of patients with Inflammatory Bowel Disease in general and for those with Ulcerative Colitis in particular. Because it was the first formulation of this family of medicines that came into the hands of the doctor. But it has not been the only biological treatment approved.
There are other active substances belonging to the group of Tumor Necrosis Factor antibodies inhibitors or TNF inhibitor drugs. This is the case of adalimumab and golimumab, as well as the biosimilars of infliximab and adalimumab.
For its part, vedolizumab is an integrin receptor antagonist drug. The objective of this active substance is to decrease the entry of inflammatory cells into the intestine. And it does that by blocking the integrins, membrane receptors that allow the passage of white blood cells and lymphocytes into the intestine.
One of the latest biologic drugs approved has been ustekinumab. In this case, it focuses on blocking the action of interleukins 12 and 23. These proteins are involved in the regulation of the inflammatory response. When they are elevated, activation and a lymphocyte proliferation occurs, which in turn provokes an inflammatory response of the organism.
Side effects of biologic treatment in Ulcerative Colitis
Usually, the side effects of biologic drugs are mild. It is common for the patients to feel tired, to experience some skin reactions, nausea, vomiting, joint or muscle pain, and fever3.
When the biologic treatment is performed by intravenous administration with infliximab, adalimumab or golimumab, the patient may report some reaction. For example, shortness of breath, hives, redness, itching and swelling of the lips and throat, or headache. If this were to happen, the infusion would be stopped in order to resume it at a slower rate. In the following administrations, the patient would be premedicated with corticosteroids.
For their part, patients treated with adalimumab or golimumab may have a skin reaction at the subcutaneous injection site.
In general, all biologic drugs can increase the chances of infection, especially respiratory infections. Therefore, health professionals recommend keeping all vaccines up to date. And, if you have any symptoms of infection such as fever or cough, it is advisable to tell your doctor.
Contact UsFor more information
Contact Us