News
World IBD day, May 19th, 2021
May 17, 2021
Events
- Given the unmet need for safer therapeutic alternatives for treating ulcerative colitis, granulocytapheresis has proven its efficacy in different clinical settings and shows an excellent safety profile.
- Dr. Eugeni Domènech, Head of the Digestive System Department at the Germans Trias i Pujol University Hospital in Badalona, is one of the authors of the article, which updates the GMA mechanism of action, recent clinical data on efficacy and safety, and practical aspects of the use of GMA in patients with ulcerative colitis from a European perspective.
Madrid, May 2021. Half of all patients with ulcerative colitis (UC) require at least one course of systemic corticosteroids in their lifetime. Approximately 75% of these patients will also need immunosuppressive drugs in the medium term to avoid colectomy. These drugs raise concerns about the increased risk of serious and opportunistic infections and cancer, especially in older patients and those with comorbidities, highlighting the unmet need for new and safer therapeutic alternatives to manage them.
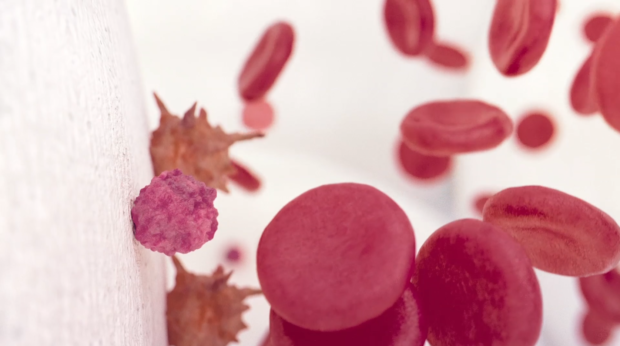
Granulocyte and monocyte apheresis (GMA), a non-pharmacological procedure (CE-marked medical device) for the treatment of ulcerative colitis (among other immune-mediated diseases), remains the only therapy targeting neutrophils, the main pathology-triggering immune cells in ulcerative colitis. This treatment involves the selective removal of activated neutrophils and monocytes from the bloodstream by passing the patient’s blood through an external column, encouraging their replacement by immature (non-activated) granulocytes and monocytes. This action reduces the migration of these cells to areas of inflammation in the colon, which in turn reduces inflammation in the tissue. In addition, passage through the column induces the secretion of anti-inflammatory cytokines, replacing the inflammatory cells retained in the column with immature cells of anti-inflammatory phenotype. Additionally, apoptotic neutrophils and monocytes returning to the bloodstream trigger the proliferation of anti-inflammatory regulatory T and B cells. All these actions induce an immune reset for an anti-inflammatory phenotype in the patient’s immune system.
In fact, this procedure has proven its efficacy in different clinical scenarios and exhibits an excellent safety profile. It is therefore a first-line therapy in Japan. However, although the treatment has been approved by the European Union since the early 2000s, it is used differently in our environment.
Use of GMA: Mechanism of action, efficacy and practical aspects
The aim of the article “Use of granulocyte/monocytapheresis in ulcerative colitis: a practical review from a European perspective” was to provide an overview of recent clinical data on GMA, its efficacy and the practical aspects of its use in ulcerative colitis from a European perspective. The article was published in the March issue of the prestigious World Journal of Gastroenterology. Among the main results, it is established that GMA is a well-tolerated treatment, with excellent patient perception, and that it also offers the possibility to treat the disease using a unique mechanism of action that compliments other drugs approved for the management of UC.
“The emergence of biological treatments for UC from 2005 onwards initially reduced interest in GMA. However, these drugs have limited efficacy in the medium term, with clinical remission rates at one year of around 30% of treated patients, a high probability of secondary loss of response and, in the case of anti-TNFs, a suboptimal safety profile. All this has rekindled interest in GMA, both as a rescue treatment and as concomitant treatment with biological drugs, given that it does not increase the risk of adverse effects”, explains Dr. Eugeni Domènech, Head of the Digestive System Department at the Germans Trias i Pujol University Hospital in Badalona and main author of this update.
Dr. Domènech regrets that GMA has become a rescue treatment after anti-TNF drugs in Europe. He calls for GMA to be “an alternative in vulnerable patients (elderly, with severe comorbidities or with a recent history of cancer)”. In addition, it raises the possibility of starting combination treatments with any of the drugs currently available in order to increase short-term efficacy.
For the future, and in the absence of robust studies to prove it, he predicts that GMA “could be a strong candidate for preventive treatment of new flares-up in at-risk patients, without increasing the risk of adverse effects of treatment”. The doctor argues that although multiple studies have been carried out over the last decade evaluating genetics, genomics (mRNA, microRNA), proteomics and even metabolomics, as well as studies based on the gut microbiota, to identify biological pathways or new therapeutic targets, the results obtained so far do not yet permit us to identify which treatments are most suitable for each patient or at each moment in time.
Contact UsFor more information
Contact Us