Monitoring nutrition and staying physically active are the two key points for leading a healthy lifestyle. Although this fact is important at any age, it is even more so if we wish to reach old age in good health conditions. The onset of conditions, such as inflammatory bowel disease (IBD), is possible during this phase, especially from the age of 60. Out of the elderly patients diagnosed with ulcerative colitis1 or Crohn’s disease for the first time, 65% are aged between 60 and 69 years; 25% between 70 and 79 years; and 10% over the age of 80.2
News
Inflammatory bowel disease in elderly patients
December 13, 2022
Patient

Inflammatory bowel diseases are often accompanied by another type of known secondary condition, such as extraintestinal manifestations (EIM), which affects the skin, eyes or joints, even though they are less common in elderly patients. There are also surgical procedures, postoperative recurrence and the onset of more aggressive or severe forms of IBD.
Malnutrition, anaemia and osteoporosis in elderly patients with IBD
Having a varied, complete, balanced diet3 in elderly patients, especially those with IBD, is fundamental but not always feasible. Issues can arise whilst chewing and swallowing due to tooth loss and decreased salivation, or can worsen the digestive process as a consequence of the reduced amount and quality of digestive secretions that, accompanied by intestinal mucosal atrophy, results in worse absorption and reduced benefit from some nutrients, mainly proteins, vitamins and minerals.
The issue of malnutrition thereforearises due to a declining diet, which causes anaemia4. Although this is not the only reason. Elderly patients with IBD can also have anaemia and malnutrition due to blood loss via the gastrointestinal tract. Hence the need for elderly patients with ulcerative colitis and Crohn’s disease to ensure they are ingesting iron-rich foods daily, notably fish, meat and eggs.
Malnutrition in elderly patients with IBD is also one of the causes for the onset of osteoporosis. Calcium, phosphorus, magnesium and vitamin D deficiencies, among other components required for bone formation, influence the loss of bone mineral density and bone weakening or fragility, thereby increasing the risk of fractures.
To prevent osteoporosis in patients over the age of 60, it is recommended to stop smoking, take the right amount of calcium and vitamin D, and exercise regularly. In fact, moderate physical activity increases bone mass and strengthens muscle. Dancing, walking, running, performing aerobic exercise, climbing stairs or lifting weights are some of the activities that the population at risk of osteoporosis should perform.
Treatment of elderly patients with IBD
The healthcare professionals’ criteria for selecting a treatment and establishing the regimen to be followed by elderly patients with ulcerative colitis or Crohn’s disease are often similar to those taken into account when determining medication for any other population group. Even the efficacy and results that can be expected from the drugs are also similar.
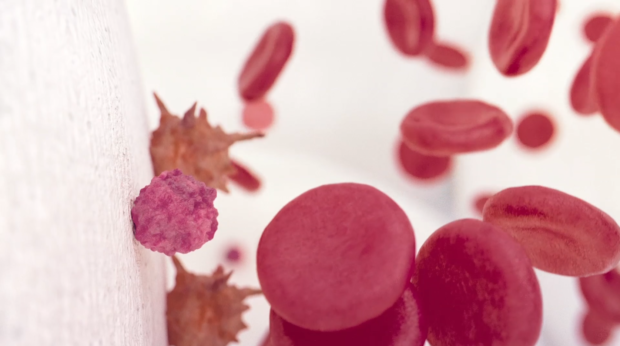
Nevertheless, when patients over the age of 60 have comorbidities, it is possible that the impact of adverse drug reactions are greater. In these cases, consultant specialists count on their therapeutic arsenal with treatment options, such as granulocyte-monocyte apheresis (GMA)5. Thanks to this non-pharmacological treatment, activated leukocytes that are responsible for intestinal inflammation are safely removed from the patient’s blood. In this way, safety is increased and risks to fragile patients, such as elderly patients, are reduced to a minimum.
Contact UsFor more information
Contact Us