- Dr. Martín de Carpi is leading a study to assess the efficacy of granulocytapheresis (GMA) in reducing the risk of loss of response to other ulcerative colitis drugs in paediatric patients.
- GMA is the only therapy targeting neutrophils, the main pathology-triggering immune cells in ulcerative colitis.
News
The challenge of treating children with ulcerative colitis: when the balance between efficacy and safety is of particular importance
June 16, 2022
Patologies

Madrid, May 2022. Although ulcerative colitis is not a common disease, if we compare it to other childhood-onset digestive diseases, it also affects the paediatric population. In fact, “this chronic disease has experienced a significant increase in incidence in children and adolescents in recent years”. So says Dr Javier Martín de Carpi, gastroenterologist at Sant Juan de Déu Hospital in Barcelona and chairman of the Spanish Society for Paediatric Gastroenterology, Hepatology, and Nutrition (SEGHNP).
This rise in cases has led to the disease being increasingly present during consultations with the paediatric gastroenterologist. In recent years, these cases are diagnosed increasingly earlier and early treatment is introduced, with all the advantages that this entails. Nevertheless, approaching this inflammatory bowel disease continues to be a challenge for the specialist. The paediatric gastroenterologist must achieve a perfect balance between efficacy and safety in the treatment he recommends to the patient.
The doctor highlights a fact that must be taken into account when choosing individualised treatment: the child is going to require treatment for very long periods of their life. However, in addition to checking that this safety profile can be maintained over time, the need to preserve certain biological processes, such as psychological growth, development and maturation, must also be assessed. “It is in our interest that these processes are not affected by the disease on its own or by the treatments that we introduce. Therefore, the approach should control inflammation and its effects rapidly, safely, and in a sustained manner. That way, we are not only taking into account that the treatment is truly effective. It is essential that it is well-tolerated and safe, and that the patient accepts and tolerates it adequately”, emphasises the paediatric gastroenterologist. Dr de Carpí warns that “some drugs can have a negative impact on children’s growth if used for a prolonged period of time (such as steroids), and others whose mechanism of action (control and alteration of the body’s defensive response and its consequences on the intestine) can determine adverse events regarding a higher risk of infections or even long-term tumours, which are fortunately uncommon”.
Granulocytapheresis: efficacy and safety
Dr. Martín de Carpi is currently leading the GUITART study: Granulocyte and monocyte/macrophage apheresis added to infliximab in paediatric patients with steroid- refractory ulcerative colitis to assess [sic] the efficacy and safety of the combined treatment, an investigation to assess the efficacy of granulocytapheresis (GMA) in reducing the risk of loss of response to other drugs. Specifically, it is infliximab biological treatment. “Infliximab is highly effective but unfortunately loses its efficacy over time in a significant percentage of patients”, he explains.
Furthermore, he is the author of the recent publication: Granulocyte and monocyte/macrophage apheresis in paediatric patients with ulcerative colitis: a case series in Spain, in a prestigious medical journal in which he presents his experience using GMA in different patient profiles in clinical practice and the results obtained, both in terms of efficacy and safety. He also details the multiple immunomodulatory effects of GMA that lead to a reduction of intestinal inflammation.
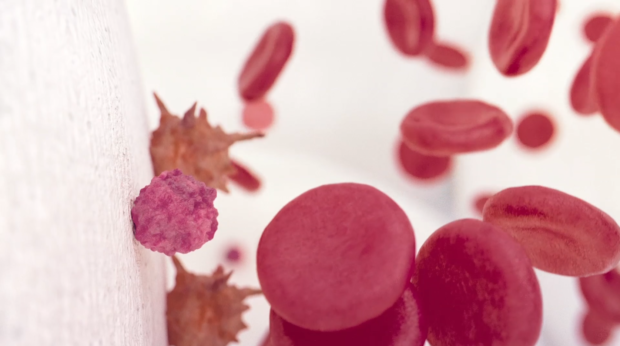
GMA is a non-pharmacological procedure for the treatment of ulcerative colitis (among other immune-mediated diseases). It is the only therapy targeting neutrophils, the main pathology-triggering immune cells in ulcerative colitis. This treatment involves the selective removal of activated neutrophils and monocytes from the bloodstream by passing the patient’s blood through an external column, encouraging their replacement by immature (non-activated) granulocytes and monocytes. This action reduces the migration of these cells to areas of inflammation in the colon, which in turn reduces inflammation in the tissue. In addition, passage through the column induces the secretion of anti-inflammatory cytokines, replacing the inflammatory cells retained in the column with immature cells of anti-inflammatory phenotype. Additionally, apoptotic neutrophils and monocytes returning to the bloodstream trigger the proliferation of anti-inflammatory regulatory T and B cells. All these actions induce an immune reset for an anti-inflammatory phenotype in the patient’s immune system.
The specialist mentions that “as the physician involved in treating these patients, the important thing to bear in mind is that some benefit can be found in each treatment”. He highlights that GMA “has proven its efficacy in different clinical scenarios and exhibits an excellent safety profile. It does not alter the patient’s immune response or other physiological processes inadequately. Furthermore, it allows the possibility of individualising treatment in terms of the technique’s frequency and duration throughout follow-up. Finally, it is a very well-tolerated technique without any relevant adverse events. The technique’s characteristics obviously require access to veins of sufficient size so that it can be performed in adequate conditions. And this is not always easy in children. It is necessary to assess each patient before prescribing and performing it”. In expert opinion, there is another advantage that promotes good adherence and acceptance of the technique: “Given the technique’s “friendly” nature (equivalent to “cleaning and purifying” blood, removing and replacing cells that act by attacking the intestine), provides added reliability and safety for the patient, which makes them trust it and its effects”.
About Adacyte
Adacyte Therapeutics is a pioneering multinational enterprise whose central headquarters is located in Barcelona. It is committed to developing and marketing unique health technologies designed to improve the health and quality of life of patients. It has been operating in Europe since 2018 and its products are currently available in over 150 university hospitals throughout Europe. The company is globally developing Granulocyte-monocyte apheresis (GMA) as a safe and effective treatment option for Inflammatory Bowel Disease (IBD) and other autoimmune diseases.
For more information, visit www.adacyte.com.
Contact UsFor more information
Contact Us